Study Links Common Gene Mutation to Increased Risk for Large Artery Stroke
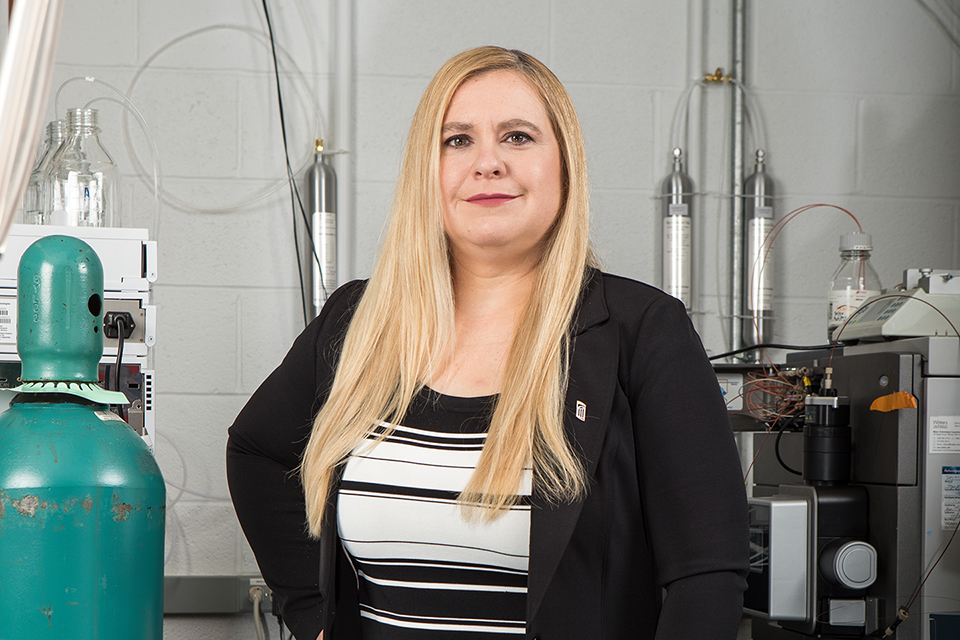
Dr. Patrick Wintrode collaborates on multinational study tracing a once-thought “silent” mutation to an increased risk for large artery stroke.
By Malissa Carroll
March 31, 2017
Patrick Wintrode, PhD, associate professor in the Department of Pharmaceutical Sciences (PSC) at the University of Maryland School of Pharmacy, recently collaborated on a large, multinational study that linked a single amino acid variant in the protein coding gene SERPINA1 to an increased risk for large artery stroke. Published in Proceedings of the National Academy of Sciences (PNAS), the study leveraged Wintrode’s expertise in hydrogen-deuterium exchange mass spectrometry to characterize the amino acid substitution, which occurs in the protein alpha-1 antitrypsin (AAT) and was previously believed to be a “silent” mutation with no association to any disease in the body.
“Previous research has shown that stroke, particularly the atherosclerotic form large artery stroke, is a highly heritable condition,” says Rainer Malik, PhD, postdoctoral researcher at the Institute for Stroke and Dementia Research at Klinikum der Universität München in Munich, Germany and lead author of the study. “However, the mechanisms surrounding how an individual’s risk for stroke is passed down from generation to generation remain unclear. The goal of this study was to identify new genes that could potentially indicate whether an individual is at an increased risk for suffering a large artery stroke during his or her lifetime.”
According to the study published by Malik and his colleagues, stroke is the leading cause of long-term disability and the second most common cause of death worldwide. The American Stroke Association reports that large artery strokes occur when a large artery feeding the brain becomes blocked. These blockages often occur as a result of atherosclerosis (hardening and narrowing of the arteries), when the plaques that contribute to the hardening and narrowing of the arteries rupture and break off to travel to another part of the body – in this instance, the brain. Malik and his colleagues note that large artery strokes exhibit the highest heritability of all stroke subtypes, with an estimated 40 to 66 percent of individuals inheriting their risk for stroke from their parents.
For this study, researchers used an innovative exome chip strategy to compare the genomes of 3,127 patients from across Europe, Australia, and South Asia who suffered a large artery stroke with the genomes of 9,778 disease-free patients. The team found two genome-wide variants: one in the gene HDAC9, an already established risk factor for large artery stroke, and another in SERPINA1. A closer inspection of SERPINA1 revealed that a single amino acid substitution in AAT placed individuals at an increased risk for experiencing a large artery stroke. Following this discovery, Malik reached out to Wintrode for assistance characterizing the substitution using hydrogen-deuterium exchange mass spectrometry.
“Although the mutation was clearly associated with an increased risk for large artery stroke, it did not appear to result in significantly impaired function or protein misfolding,” says Wintrode, whose previous research has examined AAT deficiency and been supported by organizations such as the Alpha-1 Foundation, which provides support for AAT-deficient patients. “Because my team at the School of Pharmacy has published numerous studies on AAT and other proteins in the same family, Dr. Malik and his colleagues reached out to us for assistance with comparing the mutation’s properties to the more common variant.”
At the School of Pharmacy, Wintrode’s research – which he often conducts using the cutting-edge equipment in the School’s Mass Spectrometry Center – focuses on protein folding and misfolding, as well as the role of protein dynamics in function and allosteric regulation. Although the mutated AAT displayed no structural abnormalities, Wintrode and his team – Daniel Deredge, PhD, postdoctoral fellow in PSC, and Anirudh Sivakumar, undergraduate summer research intern in PSC – found that it caused portions of the protein to become less stable. He notes that the increased structural fluctuations associated with the mutated AAT might interfere with the protein’s ability to interact with other proteins.
“Other proteins in the same family as AAT are often recruited to specific locations, such as clots or plaques, through interactions with other proteins or carbohydrates,” says Wintrode. “Concentrating these proteins at these locations enhances their function. However, in addition to being more flexible, the AAT mutation identified in this study interacts more weakly with lipoproteins than the more common variant of this gene. This could result in less AAT being concentrated at atherosclerotic plaques.”
Malik and his colleagues agree that the findings from this study emphasize the importance of every amino acid change that occurs in the body, noting that even those substitutions that do not directly influence a protein’s function can still affect the way in which those proteins interact with and bind to other molecules.
“One of the most interesting aspects of our research is that the amino acid substitution we identified commonly occurs in humans, but has never before been associated with disease,” says Malik. “We are excited to take our findings to the next level and further explore the role of AAT and AAT-neutrophil elastase (NE) complexes in the development and progression of atherosclerosis. In the future, it is our hope that drugs designed to treat patients with AAT deficiency might also be beneficial to patients who have been diagnosed with other conditions in which AAT has been shown to play an important role, including large artery stroke.”