SOP’s Coop Testifies Before U.S. Senate HELP Committee on Opioid Crisis
Testimony emphasized the need for alternative pain management treatments, and examined how pharmacists can help ensure that patients who use opioids do so safely and effectively.

By Becky Ceraul
February 13, 2019
On Feb. 12, 2019, Andrew Coop, PhD, professor in the Department of Pharmaceutical Sciences and associate dean for academic affairs at the University of Maryland School of Pharmacy, testified before the U.S. Senate Committee on Health, Education, Labor, and Pensions (HELP) as part of a hearing titled “Managing Pain During the Opioid Crisis.” Coop provided written and oral testimony during the hearing, and participated with other panelists in a lengthy question and answer session.
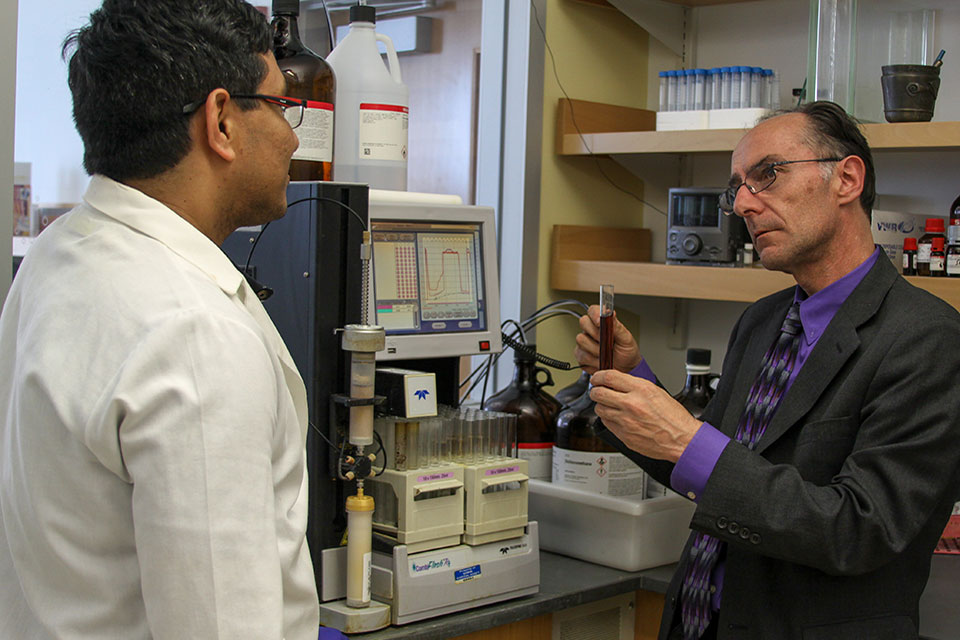
Coop’s remarks focused on his research to develop UMB 425 – an opioid painkiller with the potential for no abuse liability – and the role that pharmacists can play in helping to alleviate the opioid crisis.
His written testimony is available below. To view his oral testimony, please visit the committee hearing website here.
Written Testimony of Andrew Coop, PhD
Before the US Senate Committee on Health, Education, Labor, & Pensions
“Managing Pain During the Opioid Crisis”
Chairman Alexander, Ranking Member Murray and Committee Members, I want to thank you for the opportunity to testify today on a matter of critical importance to this country, and I applaud this Committee for continuing to seek to better understand alternatives for pain management that will not lead to opioid addiction. I am Dr. Andrew Coop and I am a professor of pharmaceutical sciences at the University of Maryland School of Pharmacy. As many of you know, the school is located at the University of Maryland, Baltimore in the City of Baltimore – a densely urban area of this country which has its share of the many challenges US cities face. The scourge of opioid addiction continues to be particularly prevalent in Baltimore despite many relatively successful efforts to lessen its impact. The University, where I have worked for 20 years, is deeply involved in this fight for our citizens’ lives. I was trained in England by John Lewis, a name that is not known to many; he was the person who developed buprenorphine, and I have followed him in my personal research efforts, focused on developing non-addictive, non-opioid alternatives for pain management to help diminish the number of individuals addicted to opioids due to chronic pain.
With this background, I want to briefly outline the current state of research in finding effective, non-addictive pain compounds, discuss the promise and to offer suggestions on strengthening the administration of pain management compounds. In the interest of transparency, I want to disclose that one of the compounds I will discuss is being developed by ALT Pharmaceuticals of which I am the co-founder along with a colleague from the School of Pharmacy, and I serve as its chief scientific officer.
Let me begin by saying that individuals who suffer from severe and chronic pain deserve our sincere sympathy. Their discomfort is debilitating and even life threatening in some cases, and their addiction to relief brought on by opioids is not by choice in most cases. We owe these individuals a better solution – one that does not come with its own complications and one that, while not curing the condition that brings the pain, enables them to return to a fuller life.
The number of individuals with chronic pain addicted to opioids is significant according to recent data. According to the CDC’s National Health Interview Survey (NHIS), an estimated 20.4% of U.S. adults – some 50 million people – had chronic pain and nearly 20 million had high-impact chronic pain – pain that frequently limits life or work activities.
Make no mistake, opioids are an outstanding class of drugs for treating pain when used appropriately. All currently approved opioids interact with and activate certain receptors in the brain which gives rise to analgesia (pain relief), and are a gold standard in treating pain when used appropriately. Unfortunately, they also give rise to all the associated side effects, including “addiction” and respiratory depression – it is the respiratory depression (slowing of breathing) that is the major cause of death on overdose. In my work and those of others in the field, we are searching for a compound that will treat the threshold of pain like opioids, but without the dependency of opioids. I attempt to avoid the term “addiction” due to the fact that it is often interpreted differently by different people, and therefore does not allow a scientific approach to the development of new opioids lacking such an effect. If we don’t know what our goal is, we will never get there. We need to define terms that can be measured biologically, namely dependence and reinforcement. They are different and have different mechanisms.
Dependence: Chronic administration of an opioid causes adaptations in the brain – specifically to the mu receptors, where they now function as if the opioid is present. On discontinuation of the opioid, the receptors are suddenly functioning without the drug that they adapted to, and this leads to withdrawal. This effect occurs no matter the reason for taking the opioid (for clinical reasons or for recreational reasons), so a patient who has received chronic administration of an opioid to treat pain will have withdrawal just as much as a person taking illicit opioids. The withdrawal effects are severe (like a bad case of the flu) and leads to patient seeking opioids to prevent withdrawal. Both prescription and illicit opioids would attenuate the withdrawal effects (as both work through mu receptors), leading to a life of drug use.
Reinforcement: In addition to analgesia, opioids also give rise to euphoria – commonly referred to as a “high”, an acute and instant effect. This effect leads to drug seeking for recreational purposes, and the drugs are usually administered through snorting or by injection for optimal reinforcement Overtime, as the individual takes opioids chronically, they develop dependence, and drug seeking turns to preventing withdrawal, rather than for reinforcement. As stated, all opioids act through the same mechanism, so prescription opioids are often diverted for recreational use due to their reinforcing properties.
My research, along with that of several others is focused on the development of an opioid lacking both reinforcement (like the abuse deterrent formulations) and dependence. Approaches include biased agonists, opioids that do not enter the brain (peripheral opioids), as well as my approach of designing a drug that activates both mu receptors and an additional biological system that prevents the side effects from mu. Many are in development in both academic and industrial laboratories, and it is critical that this research continue to be funded. The FDA has a critical role in the approval of such opioids, as we need an approach that will be both rapid in getting the drug to patients, but ensure that the new opioids are indeed safer than the current clinically approved ones. For instance, the drug developed in my laboratory appears to lack dependence in animal tests, but is reinforcing in larger rodents. Thus, although this compound (UMB 425) appears promising it is not a panacea, is only half-way to the optimal analgesic, and would almost certainly not be approved by the FDA, due to the potential for illicit use through its reinforcing properties, something that has happened recently for other new opioids.
An example of effort to create a drug for pain management without the complications of reinforcement is loxicodegol under development by an industrial laboratory.
The efforts to design a drug that would treat the same level of pain as a traditional opioid but would lack both dependence and reinforcement characteristics continue in laboratories across the US, but may take a number of years to reach the prescribing market. Like you, I wish this were not the case, but the research is intense and hopeful. A more rapid approach would be the use of drug combinations, where a lower dose of opioid is combined with another approved drug leading to lower doses of opioid required.
Research is also ongoing to find ways to potentially reduce recreational use of opioids, which is of concern to policymakers and the nation as a whole as the drug crisis continues. One approach is to focus on the use of “abuse-deterrent formulation”. For example, we can use tablets that prevent removal of the opioid to be diverted for recreational use and injected or snorted, but when taken orally will have the desired analgesic effect. The same is true for using a patch for transdermal drug induction. Taking a drug orally or transdermally leads to less reinforcing effects, as it is the rate of increase in levels that is correlated with reinforcement. Abuse deterrent formulations are strong step towards the optimal opioid, but, however, do not prevent the development of dependence as that is due to chronic, long-term action of opioid on the brain’s mu receptors – so not yet perfect.
As noted above, opioids should continue to be available to patients for the treatment of severe pain, as they are unsurpassed in their ability to treat chronic pain. That said, we need to ensure patients who require opioids are able to have them prescribed. However, their use should be reduced to a minimum, with education of patients on appropriate use and misuse. This requires a multi-faceted approach to pain management, including education of both patients and prescribers that pain is to be managed, rather than eliminated. This requires a team-based approach, where one size does not fit all. We all have experienced pain of some sort, and the first line of defense is to use aspirin, ibuprofen, acetaminophen or naproxen. When these and other over-the-counter medicines fail to relieve our symptoms, we turn to our physicians who may suggest alternative or complementary approaches such as exercise, physical therapy, weight loss, acupuncture, or cognitive behavioral therapy. There are local anesthetics and nerve blockers that are effective for surgical pain, but cost is often an obstacle. Topical capsaicins work well in many cases. Medical cannabis, controversial as it is, has potential, but well-designed studies are lacking. However, these potential sources of relief may not suffice especially for those with high-impact chronic pain and many require more patience and dedication than a pain sufferer can manage, and we ask for more. Many patients have come to expect a prescription of opioids that unrealistically totally eliminates pain when the appropriate goal is to reduce pain to a manageable level. Patient education, counseling, and follow-up care are critical to minimizing the risk of addiction.
I cannot stress enough the importance of prescriber education on opioid prescribing and would hope that this Committee and other interested bodies would continue to push for reducing the number of potentially unneeded opioid prescriptions written. Further, I suggest that patients need to take more personal responsibility for managing their pain before asking one’s physician “for something stronger”.
If I might turn to my own adopted profession and how pharmacists can contribute to reducing addiction. We are behind the counter when a prescription is filled and our prescription records often tell an important story about a particular patient. We are on the front line when opioids are the choice. The opioid epidemic requires an “all hands-on deck” inter-professional team approach to truly combat opioid-related deaths and adequately treat opioid use disorder. Adding to the complexity, mental illness and substance use disorders are often concurrent chronic disorders. We want to make you aware of the unique expertise that specialized pharmacists can bring to this effort. Pharmacists are medication experts and one of the most accessible health care professionals, yet they have been underutilized in fighting this epidemic. Expanding the prescribing of medications like buprenorphine/naloxone to include pharmacists would optimize treatment access and patient care.
Pharmacists are routinely making a difference every day by dispensing medications like naloxone and educating the public about this lifesaving antidote for opioid overdose. They receive years of training to educate patients, manage and monitor medications, including for side effects and drug interactions, and, in some cases, prescribing and administering medications. Allowing pharmacists to practice at the full extent of their education expands access to care. When pharmacists gained the authority to administer influenza vaccine and other vaccinations, immunization rates significantly increased. As a result, 280,000 pharmacists are trained to administer vaccines. Pharmacists also receive specialized training in various practice areas. For instance, psychiatric pharmacists are uniquely qualified to work with opioid use disorder patients and are experts in medication use and abuse/diversion. Psychiatric pharmacists receive graduate pharmacy degrees and post-graduate residency training in psychiatry and substance abuse. They are eligible to become board certified psychiatric pharmacists (BCPP) by completing required prerequisites and a rigorous national exam.
Most states allow pharmacists to prescribe or adjust patient medications and monitor medication effects in collaboration with a physician through laws permitting collaborative drug therapy management (CDTM) agreements. Patients with substance use disorders and mental illness often require complicated medication regimens. Collaboration between prescribers and pharmacists helps to optimize medication selection, improve safety, and expand access to care, especially in areas with a shortage of health professionals.
Buprenorphine/naloxone is an effective treatment for opioid use disorder. Unlike other medications, including prescription opioids, buprenorphine/naloxone can only be prescribed by a DATA-waivered prescriber, which limits treatment availability. Lack of institutional, mental health and psychosocial support has been cited as significant barriers to prescribing buprenorphine among primary care providers. Pharmacists are not currently eligible to apply to become DATA-waivered. We ask your support and petition for federal legislative changes which would allow pharmacists participating in CDTM agreements to prescribe buprenorphine/naloxone collaboratively with physicians to further expand access to care and improve treatment outcomes. I strongly recommend that we allow pharmacists to prescribe buprenorphine as part of an overall management of care for opioid use disorder, and gain reimbursement from Medicare. We need a long-term solution to the opioid crisis, but we also need to ensure that current patients have optimal access to medication-assisted treatment.
In conclusion, we must continue to allow access to opioids for those individuals with significant pain while we search for alternative medicines to control pain. Alternatives to opioids are within reach and research funding into such medications must not be threatened if progress is to be made. Policies designed to stem illicit drug use must not jeopardize appropriate health care. Greater efforts into the development of “safer opioids” are warranted. Prescriber and patient education on the use, and possible misuse of opioids for chronic pain conditions must continue and be strengthened. Teams addressing the opioid crisis should include pharmacists.
Thank you.