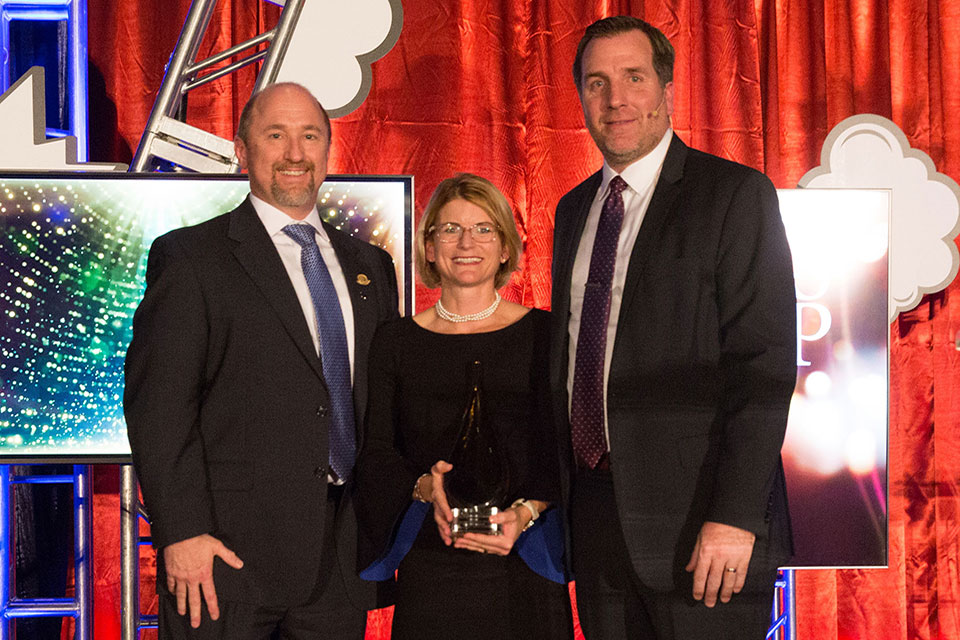
Congressman John Sarbanes Visits School of Pharmacy
Meets with dean and faculty to learn more about the School and discuss issues of importance to the profession.

By Malissa Carroll
September 11, 2013
The School of Pharmacy recently welcomed Congressman John Sarbanes for a tour and meeting with Natalie D. Eddington, PhD, FAAPS, FCP, dean and professor of the School, and Nicole Brandt, PharmD, CGP, BCPP, FASCP, associate professor in the Department of Pharmacy Practice and Science and director of clinical and educational programs for the Peter Lamy Center on Drug Therapy and Aging. During the visit, Sarbanes learned more about the School’s work with aging populations and discussed a wide range of issues currently affecting the pharmacy profession.
“The University of Maryland School of Pharmacy is training the next generation of pharmacists who will play a key role in our health care system,” said Congressman Sarbanes. “From helping to improve health outcomes to lowering health care costs by reducing the number of hospital and emergency room visits due to medication complications, well-trained pharmacists can make a huge difference in people’s lives. I have seen first-hand the dedication of students at the School of Pharmacy, and I will continue working hard to support them.”
Sarbanes was introduced to the School’s numerous academic programs, including its Doctor of Pharmacy program, graduate programs in pharmaceutical health services research and pharmaceutical sciences, online master’s degree programs in pharmacometrics and regulatory science, and four dual degree programs. “The University of Maryland School of Pharmacy is a truly comprehensive school of pharmacy,” Eddington told him.
Eddington also spoke about the School’s clinical programs, including the innovative Maryland Patients, Pharmacists, Partnerships (P3) Program. Launched in 2006, the Maryland P3 Program is a partnership of the School of Pharmacy, the Maryland Department of Health and Mental Hygiene’s Center for Chronic Disease Prevention and Control, and the Maryland Pharmacists Association. The program contracts with pharmacists to serve as medication experts working in collaboration with patients’ primary care providers to assist with proper use of medications, counseling, and overall disease state management.
“The Maryland P3 Program has a measurable impact on the clinical outcomes of participating patients,” said Eddington. “The data we have gathered from the numerous initiatives in which the program has been involved shows that patients with diabetes who are enrolled in the Maryland P3 Program have significantly higher control of their diabetes when compared to patients who were not enrolled in the program.”
Also highlighted were a number of advocacy issues of particular importance to the pharmacy profession. The progress that pharmacists have made towards advancing the profession, such as having legislation passed that permits pharmacists to administer certain vaccines to patients, was reviewed, and future challenges, such as receiving provider status, were discussed.
“At this time, pharmacists do not have provider status and are not reimbursed for the valuable services they provide to patients,” said Eddington. “As a result, we have developed unique programs, such as the Maryland P³ Program, through which reimbursement to pharmacists is possible. However, these programs are very discrete. There may be patients who would benefit from these services, but because those services are not integrated in the current model of care on a broader scale, patients are unable to access them.”
Jay A. Perman, MD, president of the University of Maryland, Baltimore, joined the meeting to provide insight on these challenges, championing a team-based approach to patient care.
“At the University of Maryland, we value interprofessional education and a team-based approach to patient care as key to ensuring that our students understand the value of their colleagues in other professions when they enter their careers,” said Perman. “However, we need funding for research to support a formal measurement of outcomes of patients who experience team-based care. We need data that clearly illustrates the outcomes, cost savings, and patient satisfaction associated with this approach.”
The meeting concluded with a presentation that spotlighted the School’s Peter Lamy Center for Drug Therapy and Aging. Brandt spoke about the Center’s commitment to improving drug therapy for aging adults and discussed its recent research efforts.
“The Peter Lamy Center for Drug Therapy and Aging is primarily focused on improving health care policy that affects the aging population,” said Brandt. “Through our educational programming partnerships with managed care and long-term care providers, we provide students, practitioners, and patients with up-to-date and accessible information on the best practices in geriatric pharmacotherapy.”
Excited about the School’s innovative programs and approach to team-based care, Sarbanes encouraged faculty to seek out new, inventive ways to connect the work being done across the different departments and schools, as well as to continue leading the way in revolutionizing patient care.