Balassone Lecture Looks at Clinical Pharmacists’ Pandemic Experiences
Faculty members in the School of Pharmacy’s Department of Pharmacy Practice and Science share their professional experiences and lessons learned during the COVID-19 pandemic.
By Malissa Carroll
February 4, 2021
The University of Maryland School of Pharmacy hosted its Francis S. Balassone Memorial Lecture in November. While this annual event is traditionally held in one of the School’s large lecture halls to accommodate the many faculty, staff, and students who gather to listen to an expert in the field of pharmacy practice share valuable insights from their clinical, teaching, or research experiences, this year was a bit different.
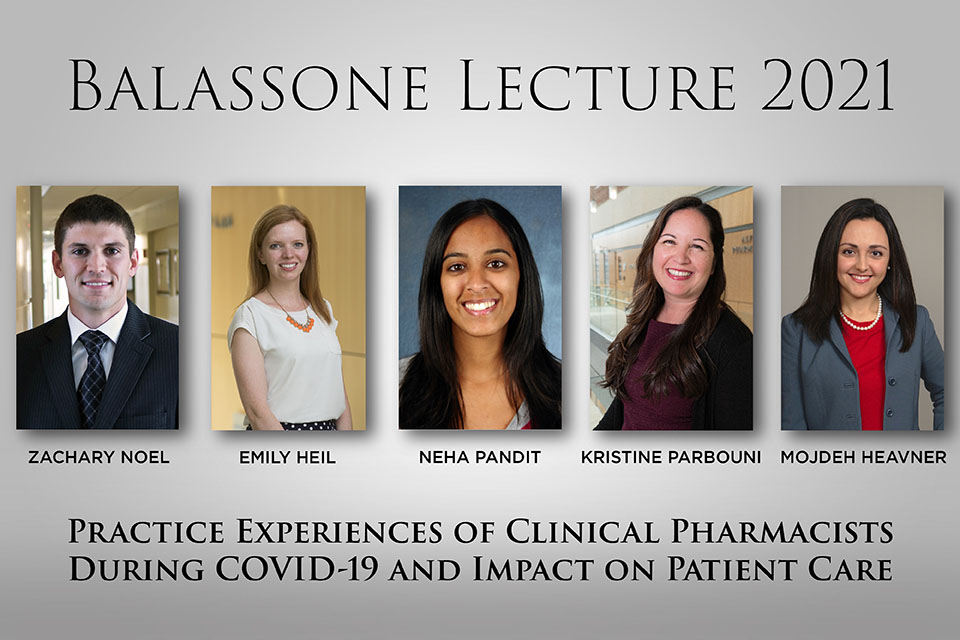
Given the School of Pharmacy’s virtual format for the fall semester, this year’s lecture was held online and featured a panel discussion that included five experts from the School of Pharmacy’s Department of Pharmacy Practice and Science (PPS). Titled “Practice Experiences of Clinical Pharmacists During COVID-19 and Impact on Patient Care,” the event spotlighted the professional experiences and lessons learned by the faculty members as their practice sites transformed and their clinical responsibilities began to evolve during the COVID-19 pandemic.
“This year’s Francis S. Balassone Memorial Lecture is special because it highlights the expertise, dedication, and accomplishments of our faculty here at the School of Pharmacy,” said Natalie D. Eddington, PhD, FCP, FAAPS, dean and professor of the School, in her opening remarks for the event. “These individuals have been on the frontlines of the COVID-19 pandemic in their roles as practitioners with the University of Maryland Medical Center (UMMC) – some intimately involved in the treatment of patients diagnosed with COVID-19, while others adjusted their roles and responsibilities to ensure continuity of care for other patients during this challenging time. All of them bring unique expertise to the health care team and demonstrate the important contributions that pharmacists make to the care of patients.”
The panel discussion was moderated by Jill A. Morgan, PharmD, BCPS, BCPPS, professor and chair of PPS, and featured speakers Mojdeh Heavner, PharmD, BCPS, BCCCP, FCCM, associate professor and vice chair for clinical services in PPS; Emily Heil, PharmD, BCIDP, BCPS-AQ ID, associate professor in PPS; Zachary Noel, PharmD, BCCP, assistant professor in PPS; Neha Sheth Pandit, PharmD, AAHIVP, BCPS, associate professor in PPS; and Kristine Parbuoni, PharmD, BCPPS, associate professor in PPS. The speakers kicked-off the lecture by describing how their respective practices changed in order to care for patients diagnosed with COVID-19.
“The hospital came to a grinding halt to focus on the pandemic,” said Heil, who serves as pharmacy director of the Antimicrobial Stewardship Program at UMMC and is the infectious diseases representative on the University of Maryland Medical System’s (UMMS) Medication Management Incident Command Team, where she is responsible for the maintenance of UMMS’s COVID-19 treatment guidelines. “Initially, there were no treatment guidelines, and as we worked to determine the most effective options for our COVID-19 patients, we were getting hit with a barrage of preprint research, anecdotes, and case reports.”
She added, “The experience was actually a wonderful reminder of how awesome and small the world of pharmacy can be. As pharmacists, we relied on each other and our professional societies, talking to others across the country who were going through similar experiences. While much of our early evidence came in the form of anecdotes, at least those anecdotes came from smart, educated people in our field.”
The speakers also addressed questions about how their service on the frontlines of the COVID-19 pandemic affected their families as well as their work with students and trainees.
“Conducting patient care visits through Zoom was an interesting experience, especially for our students, since the preceptor could not physically be with them,” said Pandit, who serves as an HIV clinical pharmacist for the University of Maryland Midtown Campus THRIVE Program and whose leadership was critical in developing protocols for medication management in patients with suspected COVID-19. “Once we could shift to a hybrid approach, we were better able to help students understand what to expect from these appointments. The students really took the experience and ran with it. They did the best they could with the tools at their disposal.”
Morgan also offered the speakers an opportunity to reflect on their experiences and provide their thoughts on what could be done differently as well as what the future might hold for their practice sites.
“It has been an incredibly challenging experience, especially in the early stages, when we had no well-established, trusted guidelines about how to best care for patients with COVID-19,” said Noel, a cardiovascular clinical pharmacy specialist at UMMC who created a system-wide protocol for the use of fibrinolytics in patients with confirmed or suspected COVID-19 presenting with ST-elevation myocardial infarction. “I think we as health care professionals were all fighting against our desire to do something, because doing nothing just feels wrong. However, it was critical that we take that step back and evaluate the literature as it became available. Yes, we want to do something, but sometimes, doing nothing is better until you have the evidence to support your decisions.”



