How the CADD Center Accelerates Drug Design
Computer modeling finds the most promising compounds and guides their transformation into drugs.
By Nala Rogers, as published in Capsule Magazine Summer 2025
September 29, 2025
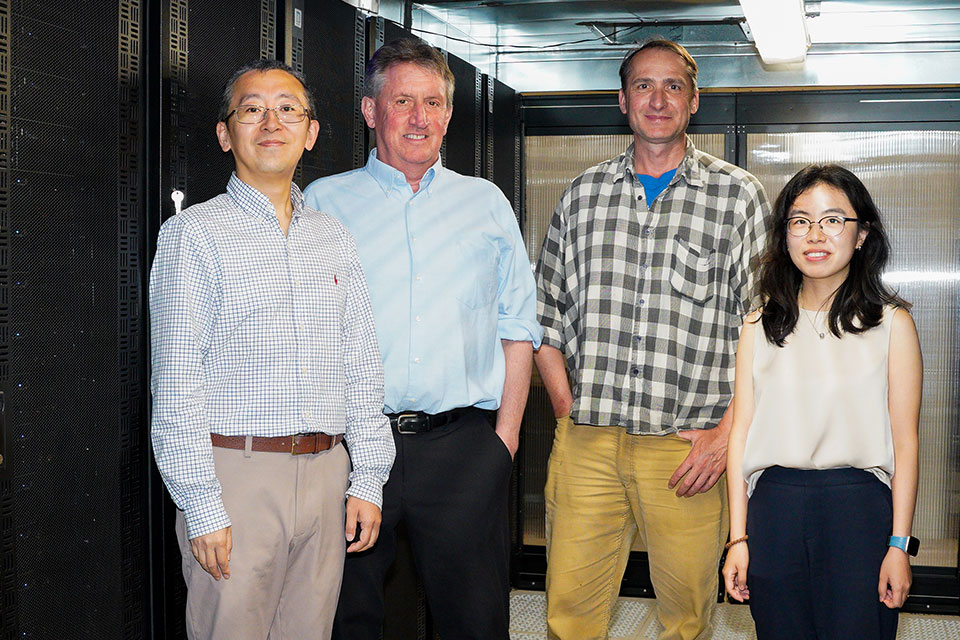
Image: From left, Wenbo Yu, Alexander MacKerell Jr., Ronald Kasl, and Yiling Nan
When structural biologist David Weber, PhD, sends a new drug target to the University of Maryland School of Pharmacy’s Computer-Aided Drug Design (CADD) Center, he imagines it being swarmed by tiny spiders.
The “spiders” are molecules such as benzene, propane, and methanol, modeled in a computer system along with the protein of interest and the water it all floats in. These mini-molecules represent fragments of larger compounds, and each type can undergo a different suite of chemical interactions. As the fragments surround the protein, computer software maps how they cling to its surface, revealing places where a new drug might bind.
This fragment-based mapping is the key innovation of the SILCS method, one of the CADD Center’s signature achievements and the foundation of its thriving spinoff company, SilcsBio LLC. The resulting “FragMaps” can be used to quickly screen millions of compounds, revealing the ones most likely to make good starting points for drugs.
“A larger drug might not be able to wiggle into a groove or a specific place, but the fragments can,” says Weber. “That, I think, has been really powerful.”
Weber is a professor of biochemistry and molecular biology at the University of Maryland School of Medicine and director of its Center for Biomolecular Therapeutics. He has worked closely with the CADD Center’s director, Alexander MacKerell Jr., PhD, the Grollman-Glick Professor in the Department of Pharmaceutical Sciences (PSC) at the School of Pharmacy, since the 1990s, before the center itself coalesced out of MacKerell’s research lab around the year 2000. At first, Weber was skeptical that MacKerell’s simulations could capture the complexity of biomolecular interactions accurately enough to be useful. Now, he is a convert — one of many across the University System of Maryland and beyond.
In the 21st century, computational modeling has emerged as a crucial component of drug discovery, and the School of Pharmacy’s CADD Center has been instrumental in its rise. Scientists and pharmaceutical companies around the world rely on methods developed at the CADD Center to save them from endless trial and error in the lab. The CADD team consists of MacKerell; the center’s co-director Jana Shen, PhD, MS, professor of PSC; Wenbo Yu, PhD, a research associate professor; and approximately 20 postdoctoral fellows, graduate students, researchers, and staff.
The center has been continuously funded since its inception, reflecting its value to medical science and society. Currently, it has eight grants from the National Institutes of Health, totaling nearly $13 million, with additional support from the U.S. Food and Drug Administration and the Samuel Waxman Cancer Research Foundation.
From Computers to Test Tubes
Work at the CADD Center includes both developing computational methodology and applying that methodology to real-life projects. Each drug development project begins with a target: a protein with a key role in a disease such as melanoma, muscular dystrophy, traumatic brain injury, or inflammatory bowel disease. A collaborator sends a new target to the CADD Center’s scientists, and they throw it to the virtual spiders, hunting for molecules that can provide a handhold with which
to steer the course of disease.
“[MacKerell] can take all those structures and do his computational magic, and say ‘these compounds are going to interact
best with the site that we want it to interact with,’” says Paul Shapiro, PhD, professor in PSC and a biochemist studying protein kinases.
Shapiro’s collaborations with the CADD Center have led to dozens of promising drug candidates, including a drug in phase 2 clinical trials that is designed to help people with acute respiratory distress syndrome (ARDS), a deadly lung condition.
Once scientists like Shapiro have tested compounds from CADD’s initial list, they send the most promising ones back to the CADD Center for ideas on how to tweak them. For instance, the models might show an unused pocket at the interface between target and proto-drug and suggest adding a particular chemical group that can reach into that pocket and grab hold more tightly.
This back-and-forth between in vitro and in silico experiments can vastly speed up drug development. Shapiro’s ARDS drug, dubbed Gen-1124, took just five years to go from a starting point compound with weak affinity for the target to an investigational drug in humans. A typical timeline is more like 10 to 15 years, says Shapiro.
Simulating the System
MacKerell hasn’t always conducted his experiments on computers. He worked with real enzymes as a graduate student at Rutgers University, earning his PhD in biochemistry in 1985 for work on how the human body breaks down alcohol. But over the next few years, first at the Karolinska Institute in Sweden and then at Harvard University and Swarthmore College, he embraced the potential of computational modeling. By the time he joined the faculty at the University of Maryland School of Pharmacy in 1993, he was one of the key figures shaping the field.
When asked to explain how it all works, MacKerell struggles to compress the complexity into mere words. The underlying models are called “force fields,” and they represent the energy between atoms.
“It’s a mathematical equation that describes the reality of the system,” says MacKerell. “You need to calculate the energy and the forces acting on a system to understand how molecules interact, which is the core of drug design.”
The applications go far beyond drug design, from materials science to chemical physics. One of MacKerell’s early papers on force fields has more than 16,000 citations because so many people have used the method.
For example, as a student, Yiling Nan, PhD, MS, used force fields developed at the CADD Center for petroleum engineering. While looking for surfactants that could help petroleum mix with water during extraction, she realized she could improve how the force fields modeled ions. Now she is working on that problem as a postdoctoral fellow in MacKerell’s lab. She wants to use her advances to improve how batteries function at different temperatures and to extend their life span by adjusting their mixture of cations, anions, and organic solvents. Better ion modeling also could help her find alternative solvents that reduce the risk of batteries catching fire.
In the late 2000s, MacKerell developed the SILCS method, which translates the modeled data into intuitive maps and practical
suggestions. SilcsBio was launched in 2012, and its customers now include approximately 30 pharmaceutical companies, including many of the world’s largest.
“What we do better than anybody else is give a really easy visualization to why certain molecules bind better than others to a given protein,” says Ken Malone, PhD, chief executive officer of SilcsBio. “The person doing drug design can see things that they couldn’t otherwise see.”
Generating the initial SILCS FragMaps can be time-consuming, but once they exist, using them is fast and computationally cheap. That’s because FragMaps simplify the details of a target protein into just the crucial information about where and how different chemical groups can bind. Competing methods such as free energy perturbation (FEP) must start from scratch to simulate how the target interacts with each compound being screened. A virtual experiment that takes a day using FEP might take a minute with a SILCS FragMap, says MacKerell.
That efficiency makes it possible to tackle problems that would otherwise be out of reach. One such project is an add-on application for the SILCS software that will model how long a given molecule stays attached to a target and what happens when it breaks away. This is called dissociation kinetics, and it is a major reason why drugs fail.
“Some drugs have a very strong affinity but can also have a very fast off-rate. So they can fall off the target very easily,” says Yu. “We want them to bind tightly, but also we want the ligand to stay there for a long time.”
Affinity, or binding strength, is defined by the fraction of molecules that are bound to their targets in a mixture, not by how long a given molecule stays attached. It’s comparatively simple to calculate affinity because you only have to model two states: fully bound or floating free. To understand the kinetics, you also have to model all the intermediate states as you drag the molecule off its target, says Yu.
That’s why drug developers normally wait to tackle kinetics until they can measure it directly. The SILCS Kinetics application could provide crucial information like the off-rate much sooner, before years and fortunes have been invested.
The Power Behind the Simulations
To perform their digital wizardry, the CADD Center scientists need vast computational power. Enter Ronald Kasl, MBA, who maintains the center’s five high-performance computing clusters with hundreds of graphics processing units (GPUs) and thousands of central processing units (CPUs). It is not typical for a school of pharmacy to have its own supercomputing center, but MacKerell realized early in his career that he would need serious hardware to run his simulations in-house. He identified Kasl, a Linux devotee, as the person to build it for him.
“Someone with Ron’s expertise and talents is essential for our work,” says MacKerell.
Kasl built the CADD Center’s High-Performance Computing (HPC) systems gradually and with minimal resources, relocating them
through a series of larger and larger rooms culminating in a state-ofthe-art data center in the basement of Pharmacy Hall. There, they run hot 24/7, roaring as they strain to keep up with demands. Icy air blasts down from ceiling vents to keep the servers cool.
Both the computing clusters and their cooling system have backup power, but once during a power outage, the backup failed. By the time Kasl arrived a few minutes later, he could feel heat radiating through the cinderblock wall as he rushed down the hallway outside. “It was like a sauna,” he says.
Even during normal operations, systems are breaking and needing to be pampered as they are pushed to the limit, a given in research computing environments. Kasl has a cardboard box full of hundreds of dead hard drives, casualties of boundary-breaking science.
Several floors up in Pharmacy Hall, Juliet Obi expresses and purifies a protein that the Dengue virus uses to replicate its genetic material. She is looking for a drug to attack this viral protein, preparing to test candidates identified through SILCS screening. The HPC clusters in the basement allow her to simulate chemical processes that would take several microseconds to play out in the real world. At conferences, she encounters envy from colleagues who are limited to much shorter simulations lasting picoseconds to nanoseconds.
“They’re like, ‘Your school has that computational power?’” she says. “I feel lucky to be here.”
Obi is a PhD candidate in Daniel Deredge’s lab, much of whose success Deredge attributes to the generosity and support of the CADD Center.
“Alex [MacKerell] actually eggs me on and pushes me to use the resources, rather than me having to ask for access or time,” says Deredge, PhD, an assistant professor in PSC.
That generosity is intrinsic to the philosophy of the ComputerAided Drug Design Center. The expertise of its scientists and the power of its computers are for the benefit of the department, and for people outside as well, says MacKerell. Kasl attributes this vision to MacKerell and, like the rest of the CADD team, he has embraced it.
“It’s unique that we have all these resources,” he says, “but it’s also unique that we are sharing them.”