Students Bridge Disciplines During Interprofessional Patient Management Competition
Dental, law, medicine, nursing, pharmacy, physical therapy, and social work students combine their knowledge and skills to better serve the needs of their patients.
By Malissa Carroll
June 6, 2016
When the members of third-year student pharmacist Joyce Yu’s team needed advice about the best medications to give a patient recently diagnosed with multiple myeloma who also suffered from complications associated with poorly treated chronic obstructive pulmonary disease (COPD), they knew where to turn. Though she had no formal clinical experience, her time as a student in the Doctor of Pharmacy (PharmD) program at the University of Maryland School of Pharmacy had equipped Yu with the knowledge to address her teammates’ questions, offering her opinions on new medications for the patient as well as re-evaluating medications that the patient had been previously prescribed.
“I knew that the medications that we prescribed needed to ensure that our patient would be able to maintain a good quality of life with the time that she had remaining,” said Yu, whose recommendation to prescribe more long-acting medications to help relieve the patient’s COPD symptoms helped her team achieve third place in the Interprofessional Patient Management Competition (IPMC) held at the School of Pharmacy in April.
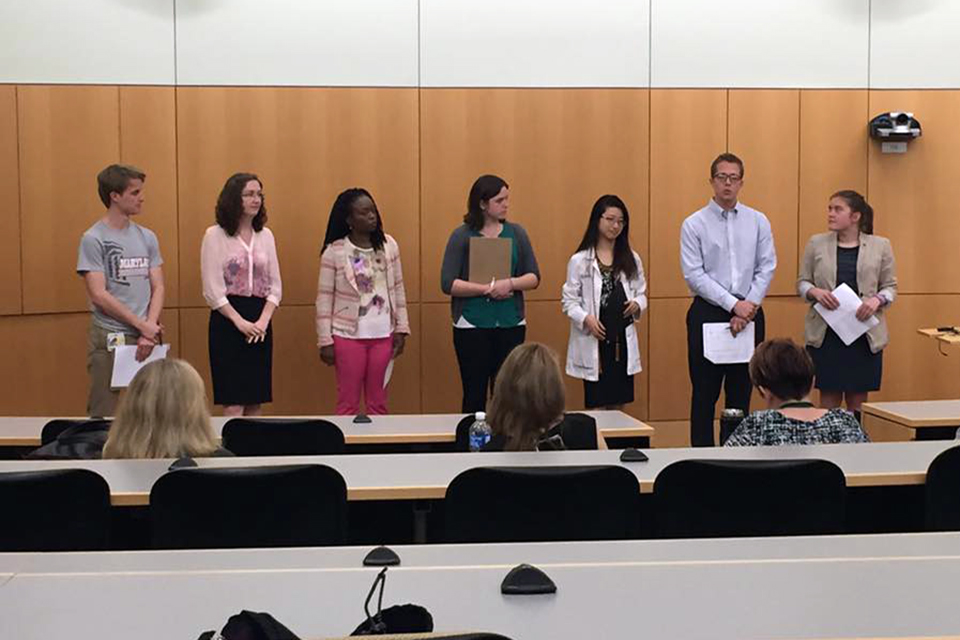
A campus-wide student competition, the IPMC features a team-based analysis of a clinical situation that is designed to help students learn to collaborate with members of other health care disciplines. All of the professional schools at the University of Maryland, Baltimore (UMB), including the Schools of Dentistry, Law, Medicine, Nursing, Pharmacy, and Social Work, were represented on each team participating in the competition.
“The IPMC helps students build the skills needed to bridge disciplines in team-based health care, allowing them to apply their current patient care knowledge to a truly interprofessional patient case,” says James Trovato, PharmD, MBA, BCOP, FASHP, associate professor in the Department of Pharmacy Practice and Science (PPS) at the School of Pharmacy and faculty advisor for the competition. “It also offers a great opportunity for students to see the knowledge and skills that other professions can bring to the table and collaborate with those professions to resolve and manage a patient’s clinical, physical, social, and legal issues.”
The annual competition is divided into two parts. Six teams participated in the first part, which involved an evaluation of a written patient case. The top three teams, as determined by the faculty who served as judges for the competition, advanced to the second part during which they were given two hours to work together to identify and develop treatment plans for the most critical issues in a new patient case created by an interprofessional team of faculty members. The teams delivered an oral presentation to the judges that explained which elements of the case they believed to be the most critical, and how they planned to resolve or manage those elements.
“It was difficult trying to determine which problem should be our team’s top priority,” says Yu. “Although our patient had a number of comorbidities, caring for her son who has autism, appeared to cause her the most concern, which helped me better understand the importance of treating the patient as a whole, and not only focusing on what is written in her medical chart. I also gained a greater appreciation for my team members’ disciplines. I could not have managed this patient without their guidance and willingness to collaborate with me.”
“The case was truly multifaceted and touched on all of the disciplines present in our interprofessional team, so everyone had a role,” adds Ha Phan, a third-year student pharmacist at the School, whose team evaluated the same clinical case presented to Yu’s team and received second place in the competition. “We reviewed the case together to identify how we could help the patient achieve the best outcome possible. I learned that having a social worker as a member of my team, especially when working with a patient from an underserved area, is essential. Every member of our team had something to contribute to ensure that we provided patient-centered care.”
The IPMC was sponsored by UMB’s Center for Interprofessional Education, and organized by the School of Pharmacy’s Student Society of Health-System Pharmacy (SSHP).



