Expanding the Range and Scope of Long-Acting Injectables
School of Pharmacy becomes a national leader for long-acting injectibles.
By Gwen Fariss Newman
April 15, 2024
In 2017, a young man in his 20s left a substance use disorder rehabilitation facility on the Eastern Shore of Maryland with a prescription for a long-acting injectable (LAI) medication. In other states, like Virginia, he could have walked into a local community pharmacy that day to have the injection administered at the pharmacy. But Maryland wasn’t yet authorizing pharmacists to administer LAIs and, while waiting for an appointment at a physician’s office for administration, the young man died.
“No pharmacist could administer it,” says Megan Ehret, PharmD, MS, BCPP, professor in the Department of Practice, Sciences, and Health Outcomes Research (P-SHOR) at the University of Maryland School of Pharmacy (UMSOP) and co-director of its Mental Health Program.
“I recall his mother saying, ‘It’s just so disheartening to think that my son died because no one could administer the medication when he needed it.’”
This man’s death would ultimately help illustrate the vital need for pharmacists in Maryland — as in most other states nationwide — to administer these long-acting drugs at the pharmacy both for the convenience of patients and to improve access to care.
“Prior to this work, pharmacists were only able to administer medications that patients could administer on their own — such as eyedrops and insulin — as well as vaccines for the flu, pneumonia, shingles, and most recently COVID-19,” says Ehret, who helped lead the legislative charge in the state for pharmacists to administer LAIs.
Long-acting injectables allow patients to switch from oral tablets taken at home to injections that last weeks or even months. They date back to 1966 with fluphenazine enanthate, an antipsychotic used to treat schizophrenia. Today, there are 13 U.S. Food and Drug Administration approved long-acting antipsychotic and three substance use disorder injectable medications, with the market expanding to include drugs for HIV, diabetes, and cholesterol.
“There’s been an explosion of these drugs in the last three years,” says Ehret.
LAIs are most often prescribed for mental illness and substance use disorders and are ideal for patients, for example, who forget to take daily medications or suffer from some of the most severe maladies as well as repercussions from missed doses.
Along with the COVID-19 pandemic came a new sense of urgency both for vaccine availability as well as for traditional health care within the physician’s office setting. Having pharmacists authorized to administer the COVID-19 vaccine was an important public health initiative that was welcomed by both physicians and the nursing community as well as by patients themselves. But receptivity to pharmacists administering LAIs wasn’t always the case. Initially there was resistance from physicians and the nursing community.
“We weren’t asking to take on the roles of physicians who prescribe these medications or nurses who administer them,” says Ehret, “but rather to serve as an added resource in a collaborative health care environment.”
Legislation for pharmacists in Maryland to administer LAIs was approved by the Maryland General Assembly in 2021 after long-term advocacy by UMSOP faculty members to state policymakers on the need for expanded pharmacist authority. Regulations were developed and approved in 2022.
Wasting No Time
Ever on the forefront, the School of Pharmacy in October 2022 promptly introduced into its Doctor of Pharmacy curriculum a course for third-year students to train them on administering LAIs.
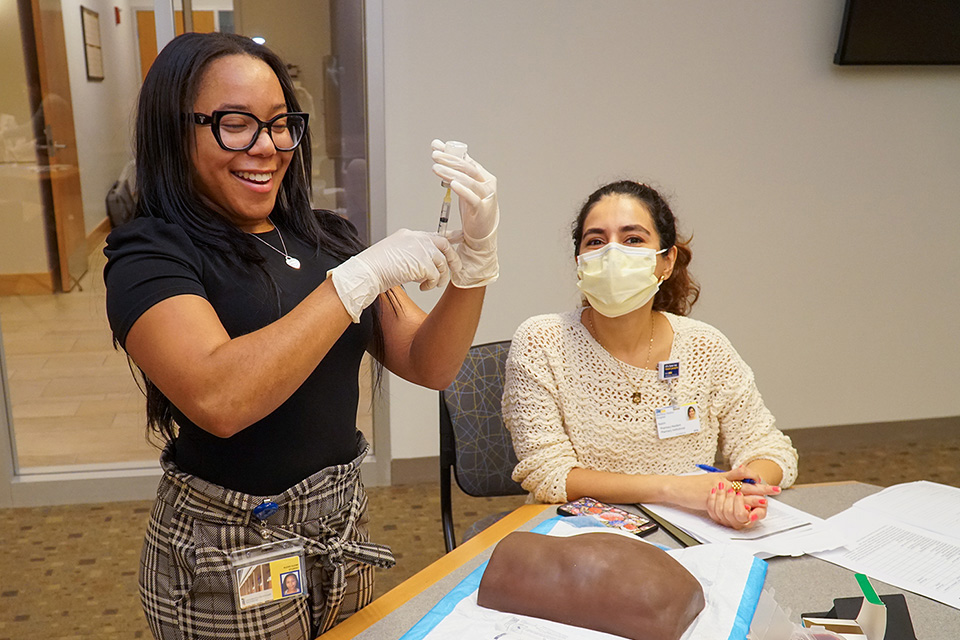
The course — the first in the state and one of the few in the country — includes a self-paced study session, a medication mixing station, and a hands-on practice lab.
UMSOP students are now taught state regulations on administering maintenance injectable medications; how to prepare the medication, including proper reconstitution, shaking and drawing up medications into syringes; gluteal injections using a simulation anatomic model; and reviewing faculty-developed case studies that allow them to role-play patient education on LAIs.
“With this curriculum, every one of our student pharmacists graduates with the ability to both prepare the medications properly and to administer them, too,” says Bethany DiPaula, PharmD ’95, BCPP, FASHP, a professor of P-SHOR and co-director of the School’s Mental Health Program along with Ehret.
The first cohort of approximately 100 trained students graduates in May.
In quick succession, a second program developed by the School of Pharmacy allows already licensed pharmacists to be certified in delivering long-acting injectables. That program consists of a home study component and a hands-on learning lab to practice reconstitution and administration. Thus far, the program has been delivered to pharmacists in Maryland at UMSOP, at the Maryland Pharmacists Association’s Annual Meeting, and at an independent pharmacy in Annapolis, all in 2023.
The objectives of the maintenance injectable medication training are to provide appropriate education to the patient regarding the injectable medication, demonstrate the preparation of the medication for injection using appropriate sterile technique and infection control procedures, and, in accordance with the product labeling, select the appropriate administration site on an anatomical model.
Other objectives include demonstrate the injection in accordance with current practice standards, document the patient information, medication, lot number, dose administered, injection site, and patient reaction, and describe methods for communicating appropriate information to the prescriber.
Spreading the Word
The School of Pharmacy’s program has been so well received that organizations such as the American Psychiatric Association, the American Association of Psychiatric Pharmacists, and the Psych Congress Nurse Practitioner Institute have requested training at their conferences and events in cities like Boston, San Diego, and New York.
“Some are organizations we’ve previously worked with,” says Ehret. “They asked, ‘You have all this equipment already … would you be willing to bring it and teach us?’”
The stars of the training?
Anatomical models of human arms and buttocks — 36 of them, in fact, that trainees use to practice the injections. “Participants walk away more confident that they understand how to do this,” says DiPaula.
UMSOP was the first school of pharmacy in Maryland to offer LAI training for students and pharmacists. The training is unique nationwide because of the hands-on components with the anatomical models. The journal Mental Health Clinician recently published an article spotlighting the success of UMSOP’s program and its evolution over a short period of time.
In its first year, close to 1,000 students, pharmacists, and other health care providers at events throughout the state and nation have participated in UMSOP’s training program for the proper administration of LAIs.
“The largest percentage of long-acting injectables are medications for mental health illness and addictions,” says DiPaula, “and for patient populations like these who are vulnerable and already have access to care issues, this is a potential solution.”
“Each state has its own nuances, and I think Maryland has addressed some patient populations that are very vulnerable and that really benefit from improved access to care,” says Ehret.
“There’s always a need for access especially in the Baltimore metro region,” she adds. “We have a manpower issue in health care nationwide, and it’s our goal locally to expand access to effective treatment — and to meet patients where they are.”
Reducing the Risk of Suicide
What are the early results of LAIs targeting vulnerable populations?
A study spotlighted in Medscape found that the suicide rate among patients with schizophrenia spectrum disorders was more than 20 times higher than that of the general population.
Several published studies show that only 40 to 60 percent of people with schizophrenia stay on track with their daily meds and that switching to a long-acting injectable antipsychotic within the first two years of a daily oral pill protocol reduced the risk for death by suicide by 47 percent.
A study from the University of California, Los Angeles showed that of patients recently diagnosed and prescribed medication, just 5 percent of those using LAIs saw a return of their symptoms, versus 33 percent taking daily oral medications.
“There is definite data demonstrating safety and effectiveness,” says DiPaula.
Ehret laments the death of the young man whose loss prompted changes in Maryland’s stance on pharmacists administering LAIs.
“Had he been able to walk into a community pharmacy in Maryland, a pharmacist could have administered an injection that might have saved his life.”
DiPaula and Ehret both specialize in psychiatric pharmacology “so this initiative is near and dear,” says DiPaula. “To design and implement a program like this is a significant milestone.
“The health care field is changing, and the role pharmacists play is as well,” she adds. “Patient care needs are changing, too. So, it makes sense that delivery options will also change. It’s exciting.”
This article originally appeared in the Spring 2024 issue of Capsule Magazine.



