UMSOP Collaborates with Johns Hopkins to Support Long COVID Patients
Collaboration highlights the vital role of pharmacists in a team-based approach to post-COVID care and recovery.

By Pam Carder
November 12, 2025
Image: Mojdeh Heavner and Erin VanMeter.
As the health care community continues to respond to the long-term effects of COVID-19, the University of Maryland School of Pharmacy (UMSOP) and the Johns Hopkins Hospital Department of Pharmacy are helping to lead the charge through a groundbreaking collaboration with the Johns Hopkins University School of Medicine.
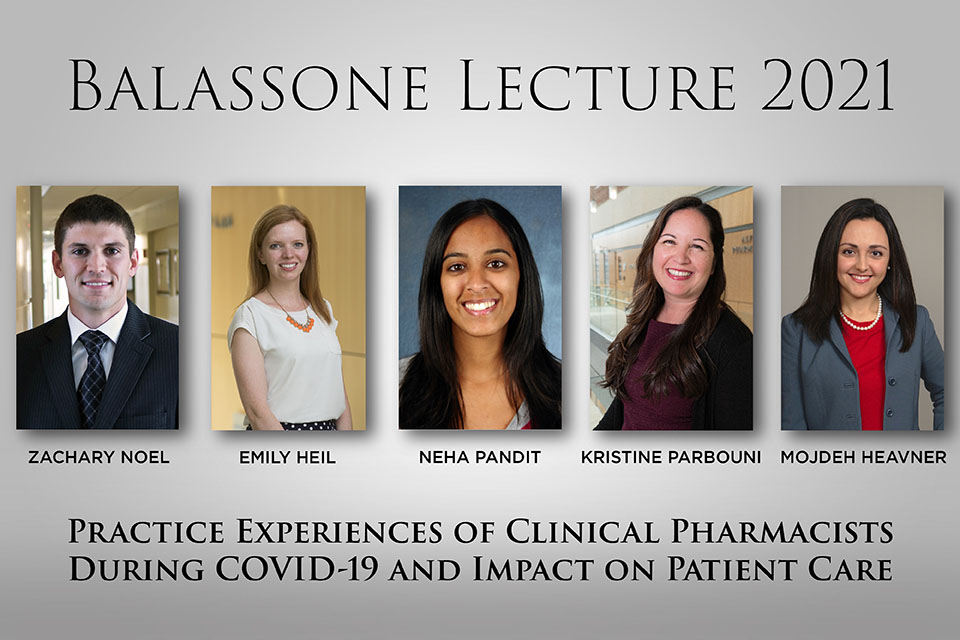
Mojdeh Heavner, PharmD, BCCCP, FCCM, FCCP, professor of practice, sciences, and health outcomes research (P-SHOR) and assistant dean for experiential learning at UMSOP, and Erin VanMeter, PharmD, BCACP, an adjunct faculty member at UMSOP and ambulatory care clinical pharmacy specialist at the Johns Hopkins Health System, serve as the two pharmacists currently working with the Johns Hopkins Post-Acute COVID-19 Team (JH PACT). The JH PACT is an interdisciplinary clinic focused on supporting COVID-19 survivors in their recovery journeys.
Since July 2024, the JH PACT program has served 574 patients, including 317 new patients, and conducted more than 4,400 patient encounters. These numbers reflect the clinic’s continued growth and underscore the ongoing need for coordinated, multidisciplinary care for individuals living with the lingering effects of COVID-19.
The collaboration between UMSOP and the JH PACT clinic began in March 2025. The clinic itself, which first opened in April 2020, was established through a joint initiative between the Division of Pulmonary and Critical Care Medicine and the Department of Physical Medicine and Rehabilitation at Johns Hopkins Medicine to provide integrated, standardized care for patients experiencing long COVID symptoms. These include fatigue, brain fog, respiratory issues, and complications related to critical illness.
The clinic is supported in part by a grant from the Agency for Healthcare Research and Quality (AHRQ). The grant, titled Supporting Patients Recovering from COVID (SPaRC), aims to expand essential clinical services for individuals living with long COVID and to build a collaborative coalition that enhances support for primary care providers.
Pharmacists like Heavner, who specializes in critical care and has previously practiced in the Medical Intensive Care Unit at the University of Maryland Medical Center, play a vital role in optimizing medication regimens for patients whose complex health needs often evolve over time.
“Our goal as pharmacists is to support patients through individualized medication management. Many of them are receiving numerous therapies, and they need careful oversight to avoid dangerous interactions and improve outcomes,” said Heavner. “We also help educate patients on how to manage their symptoms and what to expect during recovery.”
In addition to her clinical role seeing patients through population health initiatives aimed at underserved communities at Johns Hopkins, VanMeter also contributes to pharmacy education at UMSOP through teaching in chronic disease management courses and serving as a preceptor for APPE students and the School’s ambulatory care residency program. Her academic and clinical experience uniquely positions her to support patients navigating the complex, evolving challenges of long COVID.
“Being part of this team allows us to make a real impact on patients’ recovery,” said VanMeter. “As pharmacists, we’re able to offer a unique perspective on medication management that complements the work of our colleagues in medicine, nursing, and rehabilitation. It’s a true team effort focused on meeting patients where they are in their healing journey.”
Leading the program as medical director is Ann M. Parker, MD, PhD, a pulmonary and critical care medicine specialist, and assistant professor of medicine at the Johns Hopkins University School of Medicine. Parker, a 2008 graduate of the University of Maryland School of Medicine, brings a strong clinical focus on rehabilitation and recovery in post-ICU patients, including those battling the long-term effects of COVID-19. Parker also completed her residency at the University of Maryland Medical Center.
“The JH PACT clinic was created to fill a gap in care for patients experiencing persistent, life-disrupting symptoms after COVID-19,” said Parker. “Our team brings together diverse expertise, from pulmonary care and rehabilitation medicine to pharmacy, to ensure each patient receives a holistic and coordinated treatment plan.”
Kimberly Nelson, CRNP, a pulmonary nurse practitioner and one of the clinic’s primary clinicians, works alongside Parker, Heavner, and VanMeter. She takes a leading role in patient assessment, management, and care coordination.
“Every patient’s story is different. Some are just coming out of the ICU, while others are months to years along in their journey with the Post-Acute Sequelae of SARS-CoV-2 infection (PASC) and/or Post-Intensive Care Syndrome (PICS) but still struggling day to day,” Nelson explained. “That’s why our team works closely together in our multidisciplinary approach – working holistically with our patients on their mental, cognitive, and physical health.”
In addition to clinical services, which include telemedicine and in-person visits, as well as physical, occupational, speech-language therapy, and neuropsychology, the clinic also offers a free virtual support group for patients suffering from long COVID. The group provides a safe and informal space for patients to connect, share coping strategies, and combat the sense of isolation that often accompanies chronic illness.
“We’re not just treating symptoms – we’re supporting the whole person,” added Heavner. “Being part of this effort is incredibly rewarding, and I’m proud that UMSOP is contributing to such a meaningful initiative.”
“We’re proud of Dr. Heavner’s and Dr. VanMeter’s leadership and the integral role pharmacists are playing in post-COVID care,” said Jill Morgan, PharmD, BCPS, BCPPS, FNAP, professor and chair of P-SHOR. “Their work with Johns Hopkins exemplifies the power of interdisciplinary teamwork in improving patient outcomes.”