Pharmacy Trainee Wins Award for Translational Research
Award winning research focuses on translational drug model to improve outcomes in patients with hepatitis C
By Steve Berberich
December 9, 2010
University of Maryland School of Pharmacy researchers have developed a mathematical model that may change the way doses of the hepatitis medication ribavirin are determined for individual patients. The work also helps explain why African-American patients tend to not respond as well to the drugs as other patients.
The research poster “Population Pharmacodynamic Model in Patients with Chronic Hepatitis C Virus Genotype 1,” by postdoctoral fellow Runyan Jin, MD, PhD, won the 2010 Wayne A. Colburn Memorial Award at the American College of Clinical Pharmacology annual meeting.
Hepatitis C is a serious liver disease caused by the hepatitis C virus and if not treated can lead to liver cancer and death. African-Americans have a higher incidence of the disease and death from liver cancer.
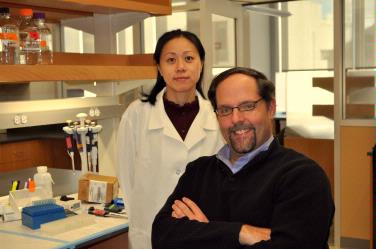
Jin analyzed 900 blood samples for ribavirin content from 400 patients enrolled in a multi-center trial to determine why hepatitis therapy works for some patients, but not others. She couldn’t have started with a better study, says Thomas Dowling, PharmD, PhD, an associate professor of pharmacy practice and science and Jin’s mentor. The blood samples were stored by the National Institutes of Health (NIH) from the milestone 2006 study, Viral Resistance to Antiviral Therapy of Chronic Hepatitis C study [VIRAHEPC], funded by NIH’s National Institute of Diabetes and Digestive and Kidney Diseases. One of the main purposes for the VIRAHEPC was the underrepresentation of African-Americans in previous studies. It used patients from eight clinics nationwide, including the University of Maryland Medical Center, under principal investigator Charles Howell, MD, professor and director of hepatology research in the University of Maryland School of Medicine.
The therapy, consisting of the anti-virus drug ribavirin, along with injections of the protective protein interferon, cures hepatitis C in some patients within six months due to a sustained viral response [SVR], suppressing the virus to undetectable levels for an extended period of time.
“Our question was why some patients in the large trial did not get this SVR cure. The response rate of African-American patients was about half that of non-African-Americans,” says Dowling, who is also co-director of the School’s Clinical Pharmacology Unit.
Jin, who is already a pediatrician, discovered that blood from the African-American patients contained lower levels of the ribavirin drug than non-African-American patients on the same therapy. Especially in early stages of the therapy, the ribavirin was not getting into the blood system as efficiently in African-Americans as in Caucasians. The mathematical model showed that the African-Americans had a pharmacokinetic difference related to the distributional volume, which means the space where the drug moves, says Dowling.
Jin hopes that her research on anti-virus mediations and how they work in different people, called pharmacodynamics, will also be useful in treating children. “It is especially important for children to get the correct dosages for safe and effective treatments.”
“I was very lucky,” says Jin. “When I was a second year PhD student, I was looking for a research project in population pharmacokinetics, and Drs. Dowling and Howell were collaborating on hepatitis C research.” She applied a mathematical method called Bayesian statistics to evaluate the relationships between the drug and SVR rates in the 400 patients in the 2006 study, a method taught to her by Michael Fossler, PharmD, PhD, an alum of the School of Pharmacy who is now director of clinical pharmacology modeling and simulation with drug maker GlaxoSmithKline.
“Runyan pulled a very nice story together with direct clinical applications. What we are faced with now [in drug development] is studies that are so very expensive, says Fossler. “Bayesian methodology helps us cut our losses and saves some patients from taking drugs that don’t work sometimes.”
Jin has completed her training at the School of Pharmacy and has accepted a position at the U.S. Food and Drug Administration. In her new career, she says, “I want to be an expert in this area of quantitative clinical pharmacology.”
